
Rewatch the Webinar
IEC 623661 Essentials: Elevating User Safety in Medical Devices
- Session Recording: 1h20
Usability engineering, also known as human factors engineering, plays an essential role in minimizing use-related risks associated with medical devices. The standard IEC 62366-1 offers valuable guidelines for integrating this discipline into the development process.
- What usability engineering activities should be included in the medical device development process?
- What are the benefits for the product?
Senior Human Factors Specialist, Maude Leclerc-De Guire, and Quality Assurance Manager, Jean-Yves Pairet, recently shared their expertise in a webinar hosted in partnership with Greenlight Guru.
After reviewing the applicable regulatory framework, they detailed the key activities involved in usability engineering at every stage of development, from identifying user needs to conducting validation testing.
Key Activities Throughout the Medical Device Development Process
Integrating usability and human factors engineering into the medical device development process is crucial for ensuring that products are safe and effective.
1. Planning Phase
2. Definition Phase
Key user needs, potential usability errors, and the use environment are identified. These insights are then translated into design inputs related to the user interface.
3. Design Phase
4. Verification Phase
Activities are conducted to ensure that the user interface design strictly complies with all specified requirements.
5. Validation Phase
1. Planning Phase
First and foremost, the human factors team draws up the usability plan, which is integrated into the design and development plan. This document details the main human factors activities, such as usability specifications, usability risk analysis, user interface specifications, as well as formative and summative evaluations.
It also defines the roles and responsibilities of all team members involved, including close collaboration between human factors specialists, user interface (UI) designers, industrial designers, and the quality assurance team.
2. Definition Phase
User Needs Definition
Defining user needs is a fundamental step in the development of any medical device. This crucial phase guides all subsequent development activities and begins with the establishment of clear use specifications.
- Clarification of the device's intended use.
- Identification of users and patients.
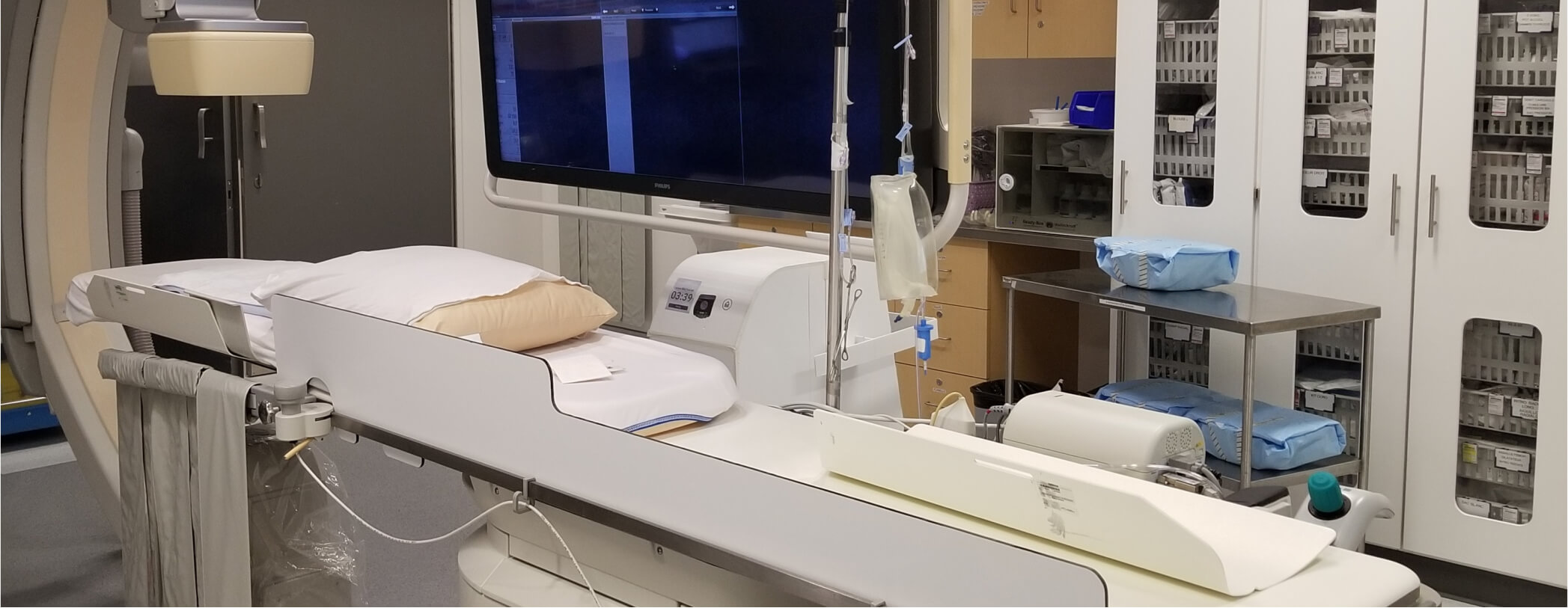
- Understanding the use environment.
Several methods are used to draft these use specifications:
- Market research, which includes analysis of competitors’ devices and documentation.
- User research, involving direct interaction with potential users of the device.
- Field observations and interview sessions with subject matter experts to gather information on the actual context of use.
Concurrently with the definition of use specifications, the Human Factors (HF) and Quality Assurance (QA) teams begin to collect and analyze existing information on known use risks. To accomplish this, they use databases such as MAUDE and GUDID, as well as internal company databases that contain complaints and CAPA reports. This activity forms the foundation for the use-related risks analysis.
Design Inputs Definition
While user needs can be vague and qualitative, design inputs should be more detailed, specific and quantitative, as they directly influence the user interface design.
2. Use-Related Risk Analysis (URRA)
3. Design Phase
Formative Evaluations
The guiding principle here is simple: when in doubt, test!
To gain meaningful insights for improving the medical device, the optimal number of participants is 5 to 8 per evaluation.
4. Verification Phase
In the medical device development process, the verification phase ensures that the user interface strictly complies with all design requirements.
- Test scenarios
- Expert reviews
- Cognitive walkthrough
- Surveys
It’s important to differentiate between formative evaluations and verification activities. Formative evaluations are iterative tests conducted during the design phase to refine the user interface. Verification, on the other hand, occurs once the device design is finalized.
Therefore, formative evaluations help identify issues and implement changes early in the development cycle, whereas verification is performed on the final design, which will undergo little to no further changes. It’s worth noting that verification should be planned early in the design phase to ensure smoother execution.
5. Validation Testing
This phase validates the user interface, focusing specifically on safety aspects related to use. Whether or not it is carried out depends on the regulatory strategy and product class.
Summative Evaluation
More specifically, summative evaluation verifies the effectiveness of all risk control measures. Its aim is to demonstrate that the device not only meets the required safety standards, but also functions effectively in the hands of users. To achieve this, the summative evaluation must accurately reflect actual use conditions.
This phase validates the user interface, focusing specifically on safety aspects related to use. It may or may not be conducted, depending on the regulatory strategy and the product class.
- Prioritize critical and essential tasks.
- Test in the actual user environment.
- Select an adequate sample of users (at least 15 users from each user group).
- Allow time for learning decline, especially if user training is planned.

The Benefits of Integrating Usability Engineering into Medical Device Development
Considering human factors and usability in medical device development not only helps to meet regulatory requirements but also reduces errors and use-related risks.
- Better cost and time management in the development process.
- Easier, faster and safer onboarding.
- Reduced need for ongoing technical support.
- Higher utilization rates.
- Increased sales and revenues.
- Stronger regulatory records.
Integrating usability and human factors engineering into medical device development is a rigorous process that improves overall product quality. This approach ensures that the medical device is more user-friendly, easier to operate, and more ergonomic.